The absence industry is fraught with a diverse array of leaves, ranging from simple time off to care for a loved one, to complex absences requiring coordination of disability, statutory, federal, and state leave guidance to cover any number of possible outcomes. These complex cases often require resources with a greater claim and leave management knowledge to help front-line managers assess which claims may requires a more hands-on approach. Unfortunately, modern-day absence management systems are not always prepared to help identify case complexity and thus, provide value to the administrator or its clients. The downside of a runaway complex case has implications in longer leave duration, unnecessary benefit payments, and inappropriate work allocations, to name just a few.
I saw this firsthand years ago, when I worked as an operations manager overseeing multiple claims teams. I often discussed situations where the client felt that a more hands-on approach to claims handling could have helped with an early return-to-work intervention, a better transition for the employee, or even prevented a claim from going to litigation. Those were the claims that would appear to spiral out of control quickly. When reviewing their history, it was easy in retrospect to spot the red flags. However, for a case manager with dozens of cases crossing their desk at any given time, those flags were not easily visible or even actionable. Having a tool to identify at-risk claims or those with the potential to go beyond a reasonable duration would have saved time and prevented those difficult client calls.
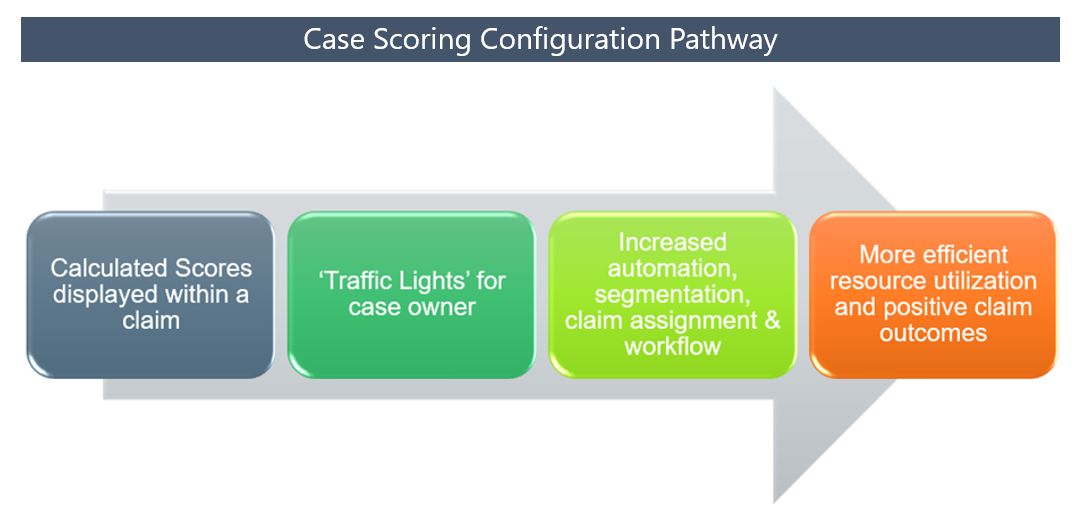
Today, FINEOS Insight helps clients address the numerous pain points resulting from unidentified complex claim behaviors using machine learning and algorithm-driven case scoring. Implementing the case scoring system allows FINEOS software users to do the following:
- Set specific parameters to determine complexity scores which will route the leave request to a more skilled claims handler. This approach allows for early resource intervention and the best use of high-value staff and their unique skill sets. This can accelerate the use of automation for low-risk and low-complexity claims, improving customer experience by reducing required touchpoints and potentially automating the adjudication decision.
- Identify claims with high cost potential. Once identified, the administrator can institute internal claims-handling procedures to target early return-to-work intervention and educational programs to impact absence durations. The leave administrator can also partner with the client’s health and wellness benefit administrator. Identifying complex claims that overlap with a client’s health and wellness program criteria allows for increased engagement and improved supplemental health claim utilization.
- Inform the claims handler of key characteristics which can drive leave complexity. FINEOS analytics focuses on a few of the most critical components, such as the employee’s occupation, work state, late claim filing, eligibility for multiple plans or benefits, coverage type and number of extension requests. For example, a one-week continuous unpaid leave for care of a family member requested in advance can be classified as having high integrity, resulting in a low complexity score. Conversely, a single intermittent absence period request made three months after the initial absence in a state which offers paid leave benefits will have significantly reduced integrity, resulting in a higher complexity score.
Using the scoring configuration feature, clients can change the calculation parameters, control claim routing, and provide resource alignment to obtain the most effective case management at the time when the claim needs it the most. Over time, the application of these methods can impact claim durations, leading to direct employer savings.
Lastly, by focusing on applying the right resource at the right time, the employee will have a more positive claim experience. While claim handlers can visually identify leaves that are trending toward complexity and take appropriate action, employees will be the recipients of quality claims management and engagement in their employer’s health and wellness programs. The combination can assist the employee with residual effects of their time away from work, while the employer will see an increase in use of fringe benefits that are often underutilized.
If you’re ready to join the FINEOS clients who have access to the complexity scoring feature, contact FINEOS today.